'via Blog this'
Stem cell
From Wikipedia, the free encyclopedia
| Stem cell | |
|---|---|
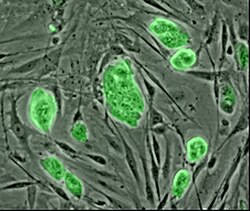 | |
| Mouse embryonic stem cells with fluorescent marker | |
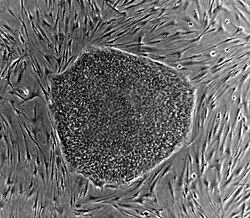 | |
| Human embryonic stem cell colony on mouse embryonic fibroblast feeder layer | |
| Latin | cellula precursoria |
| Code | TH H2.00.01.0.00001 |
This article is about the cell type. For the medical therapy, see Stem Cell Treatments.
Stem cells are biological cells found in all multicellular organisms, that can divide (throughmitosis) and differentiate into diverse specialized cell types and can self-renew to produce more stem cells. In mammals, there are two broad types of stem cells: embryonic stem cells, which are isolated from the inner cell massof blastocysts, and adult stem cells, which are found in various tissues. In adult organisms, stem cells and progenitor cells act as a repair system for the body, replenishing adult tissues. In a developing embryo, stem cells can differentiate into all the specialized cells (these are called pluripotent cells), but also maintain the normal turnover of regenerative organs, such as blood, skin, or intestinal tissues.
There are three sources of autologous adult stem cells: 1) Bone marrow, which requires extraction by harvesting, that is, drilling into bone (typically the femur or iliac crest), 2) Adipose tissue (lipid cells), which requires extraction by liposuction, and 3) Blood, which requires extraction through pheresis, wherein blood is drawn from the donor (similar to a blood donation), passed through a machine that extracts the stem cells and returns other portions of the blood to the donor. Stem cells can also be taken from umbilical cord blood. Of all stem cell types, autologous harvesting involves the least risk. By definition, autologous cells are obtained from one's own body, just as one may bank his or her own blood for elective surgical procedures.
Highly plastic adult stem cells are routinely used in medical therapies, for example bone marrow transplantation. Stem cells can now be artificially grown and transformed (differentiated) into specialized cell types with characteristics consistent with cells of various tissues such as muscles or nerves through cell culture. Embryonic cell lines and autologous embryonic stem cells generated through therapeutic cloning have also been proposed as promising candidates for future therapies.[1] Research into stem cells grew out of findings by Ernest A. McCulloch and James E. Till at the University of Toronto in the 1960s.[2][3]
Contents[hide] |
Properties
The classical definition of a stem cell requires that it possess two properties:
- Self-renewal: the ability to go through numerous cycles of cell division while maintaining the undifferentiated state.
- Potency: the capacity to differentiate into specialized cell types. In the strictest sense, this requires stem cells to be either totipotent or pluripotent—to be able to give rise to any mature cell type, although multipotent or unipotent progenitor cells are sometimes referred to as stem cells. Apart from this it is said that stem cell function is regulated in a feed back mechanism.
Self-renewal
Two mechanisms to ensure that a stem cell population is maintained exist:
- Obligatory asymmetric replication: a stem cell divides into one father cell that is identical to the original stem cell, and another daughter cell that is differentiated
- Stochastic differentiation: when one stem cell develops into two differentiated daughter cells, another stem cell undergoes mitosis and produces two stem cells identical to the original.
Potency definitions
Main article: Cell potency
Potency specifies the differentiation potential (the potential to differentiate into different cell types) of the stem cell.[4]
- Totipotent (a.k.a. omnipotent) stem cells can differentiate into embryonic and extraembryonic cell types. Such cells can construct a complete, viable organism.[4] These cells are produced from the fusion of an egg and sperm cell. Cells produced by the first few divisions of the fertilized egg are also totipotent.[5]
- Pluripotent stem cells are the descendants of totipotent cells and can differentiate into nearly all cells,[4] i.e. cells derived from any of the threegerm layers.[6]
- Multipotent stem cells can differentiate into a number of cells, but only those of a closely related family of cells.[4]
- Oligopotent stem cells can differentiate into only a few cells, such as lymphoid or myeloid stem cells.[4]
- Unipotent cells can produce only one cell type, their own,[4]but have the property of self-renewal, which distinguishes them from non-stem cells (e.g., muscle stem cells).
Identification
The practical definition of a stem cell is the functional definition—a cell that has the potential to regenerate tissue over a lifetime. For example, the defining test for a bone marrow or hematopoietic stem cell (HSC) is the ability to transplant one cell and save an individual without HSCs. In this case, a stem cell must be able to produce new blood cells and immune cells over a long term, demonstrating potency. It should also be possible to isolate stem cells from the transplanted individual, which can themselves be transplanted into another individual without HSCs, demonstrating that the stem cell was able to self-renew.
Properties of stem cells can be illustrated in vitro, using methods such as clonogenic assays, in which single cells are assessed for their ability to differentiate and self-renew.[7][8] Stem cells can also be isolated by their possession of a distinctive set of cell surface markers. However, in vitro culture conditions can alter the behavior of cells, making it unclear whether the cells will behave in a similar manner in vivo. There is considerable debate as to whether some proposed adult cell populations are truly stem cells.
Embryonic
Main article: Embryonic stem cell
Embryonic stem (ES) cell lines are cultures of cells derived from the epiblast tissue of the inner cell mass (ICM) of a blastocyst or earlier morula stage embryos.[9] A blastocyst is an early stageembryo—approximately four to five days old in humans and consisting of 50–150 cells. ES cells arepluripotent and give rise during development to all derivatives of the three primary germ layers: ectoderm, endoderm and mesoderm. In other words, they can develop into each of the more than 200 cell types of the adult body when given sufficient and necessary stimulation for a specific cell type. They do not contribute to the extra-embryonic membranes or the placenta. The endoderm is composed of the entire gut tube and the lungs, the ectoderm gives rise to the nervous system and skin, and the mesoderm gives rise to muscle, bone, blood—in essence, everything else that connects the endoderm to the ectoderm.
Nearly all research to date has made use of mouse embryonic stem cells (mES) or human embryonic stem cells (hES). Both have the essential stem cell characteristics, yet they require very different environments in order to maintain an undifferentiated state. Mouse ES cells are grown on a layer of gelatin as an extracellular matrix (for support) and require the presence of leukemia inhibitory factor (LIF).[10] Human ES cells are grown on a feeder layer of mouse embryonicfibroblasts (MEFs) and require the presence of basic fibroblast growth factor (bFGF or FGF-2).[11] Without optimal culture conditions or genetic manipulation,[12] embryonic stem cells will rapidly differentiate.
A human embryonic stem cell is also defined by the expression of several transcription factors and cell surface proteins. The transcription factors Oct-4, Nanog, and Sox2 form the core regulatory network that ensures the suppression of genes that lead to differentiation and the maintenance of pluripotency.[13] The cell surface antigens most commonly used to identify hES cells are the glycolipids stage specific embryonic antigen 3 and 4 and the keratan sulfate antigens Tra-1-60 and Tra-1-81. The molecular definition of a stem cell includes many more proteins and continues to be a topic of research.[14]
There are currently no approved treatments using embryonic stem cells. The first human trial was approved by the US Food and Drug Administration in January 2009.[15] However, the human trial was not initiated until October 13, 2010 in Atlanta for spinal injury victims. On November 14, 2011 the company conducting the trial announced that it will discontinue further development of its stem cell programs.[16] ES cells, being pluripotent cells, require specific signals for correct differentiation—if injected directly into another body, ES cells will differentiate into many different types of cells, causing a teratoma. Differentiating ES cells into usable cells while avoiding transplant rejection are just a few of the hurdles that embryonic stem cell researchers still face.[17] Many nations currently have moratoria on either ES cell research or the production of new ES cell lines. Because of their combined abilities of unlimited expansion and pluripotency, embryonic stem cells remain a theoretically potential source for regenerative medicine and tissue replacement after injury or disease.
Fetal
The primitive stem cells located in the organs of fetuses are referred to as fetal stem cells.[18]
Adult
Main article: Adult stem cell
Also known as somatic (from Greek Σωματικóς, "of the body") stem cells and germline (giving rise to gametes) stem cells, they can be found in children, as well as adults.[19]
Pluripotent adult stem cells are rare and generally small in number but can be found in a number of tissues including umbilical cord blood.[20] A great deal of adult stem cell research to date has had the aim of characterizing the capacity of the cells to divide or self-renew indefinitely and their differentiation potential.[21] In mice, pluripotent stem cells are directly generated from adult fibroblast cultures. Unfortunately, many mice do not live long with stem cell organs.[22]
Most adult stem cells are lineage-restricted (multipotent) and are generally referred to by their tissue origin (mesenchymal stem cell, adipose-derived stem cell, endothelial stem cell, dental pulp stem cell, etc.).[23][24]
Adult stem cell treatments have been successfully used for many years to treat leukemia and related bone/blood cancers through bone marrow transplants.[25] Adult stem cells are also used in veterinary medicine to treat tendon and ligament injuries in horses.[26]
The use of adult stem cells in research and therapy is not as controversialas the use of embryonic stem cells, because the production of adult stem cells does not require the destruction of an embryo. Additionally, in instances where adult stem cells are obtained from the intended recipient (an autograft), the risk of rejection is essentially non-existent. Consequently, more US government funding is being provided for adult stem cell research.[27]
An extremely rich source for adult mesenchymal stem cells is the developing tooth bud of the mandibular third molar.[28] The stem cells eventually form enamel (ectoderm), dentin, periodontal ligament, blood vessels, dental pulp, nervous tissues, and a minimum of 29 different end organs. Because of extreme ease in collection at 8–10 years of age before calcification and minimal to no morbidity, these will probably constitute a major source of cells for personal banking, research and current or future therapies. These stem cells have been shown capable of producing hepatocytes.[citation needed]
Amniotic
Multipotent stem cells are also found in amniotic fluid. These stem cells are very active, expand extensively without feeders and are not tumorigenic. Amniotic stem cells are multipotent and can differentiate in cells of adipogenic, osteogenic, myogenic, endothelial, hepatic and also neuronal lines.[29] All over the world, universities and research institutes are studying amniotic fluid to discover all the qualities of amniotic stem cells, and scientists such as Anthony Atala[30][31] andGiuseppe Simoni [32][33][34] have discovered important results.
Use of stem cells from amniotic fluid overcomes the ethical objections to using human embryos as a source of cells. Roman Catholic teaching forbids the use of embryonic stem cells in experimentation; accordingly, the Vatican newspaper "Osservatore Romano" called amniotic stem cells "the future of medicine".[35]
It is possible to collect amniotic stem cells for donors or for autologuous use: the first US amniotic stem cells bank [36][37] was opened in 2009 in Medford, MA, by Biocell CenterCorporation [38][39][40] and collaborates with various hospitals and universities all over the world.[41]
Induced pluripotent
Main article: Induced pluripotent stem cell
These are not adult stem cells, but rather adult cells (e.g. epithelial cells) reprogrammed to give rise to pluripotent capabilities. Using genetic reprogramming with protein transcription factors, pluripotent stem cells equivalent to embryonic stem cells have been derived from human adult skin tissue.[42][43][44] Shinya Yamanaka and his colleagues at Kyoto University used the transcription factors Oct3/4, Sox2, c-Myc, and Klf4[42] in their experiments on cells from human faces.Junying Yu, James Thomson, and their colleagues at the University of Wisconsin–Madison used a different set of factors, Oct4, Sox2, Nanog and Lin28,[42] and carried out their experiments using cells from human foreskin.
As a result of the success of these experiments, Ian Wilmut, who helped create the first cloned animal Dolly the Sheep, has announced that he will abandon somatic cell nuclear transfer as an avenue of research.[45]
Frozen blood samples can be used as a source of induced pluripotent stem cells, opening a new avenue for obtaining the valued cells.[46]
Lineage
Main article: Stem cell line
To ensure self-renewal, stem cells undergo two types of cell division (see Stem cell division and differentiation diagram). Symmetric division gives rise to two identical daughter cells both endowed with stem cell properties. Asymmetric division, on the other hand, produces only one stem cell and a progenitor cell with limited self-renewal potential. Progenitors can go through several rounds of cell division before terminally differentiating into a mature cell. It is possible that the molecular distinction between symmetric and asymmetric divisions lies in differential segregation of cell membrane proteins (such as receptors) between the daughter cells.[47]
An alternative theory is that stem cells remain undifferentiated due to environmental cues in their particular niche. Stem cells differentiate when they leave that niche or no longer receive those signals. Studies in Drosophila germarium have identified the signals decapentaplegic and adherens junctions that prevent germarium stem cells from differentiating.[48][49]
Main article: Induced Pluripotent Stem Cell
The signals that lead to reprogramming of cells to an embryonic-like state are also being investigated. These signal pathways include several transcription factors including the oncogene c-Myc. Initial studies indicate that transformation of mice cells with a combination of these anti-differentiation signals can reverse differentiation and may allow adult cells to become pluripotent.[22] However, the need to transform these cells with an oncogene may prevent the use of this approach in therapy.
Challenging the terminal nature of cellular differentiation and the integrity of lineage commitment, it was recently determined that the somatic expression of combined transcription factors can directly induce other defined somatic cell fates; researchers identified three neural-lineage-specific transcription factors that could directly convert mouse fibroblasts (skin cells) into fully functional neurons. This "induced neurons" (iN) cell research inspires the researchers to induce other cell types implies that all cells are totipotent: with the proper tools, all cells may form all kinds of tissue.[50]
Treatments
Main article: Stem cell treatments
Medical researchers believe that stem cell therapy has the potential to dramatically change the treatment of human disease. A number of adult stem cell therapies already exist, particularly bone marrow transplants that are used to treatleukemia.[52] In the future, medical researchers anticipate being able to use technologies derived from stem cell research to treat a wider variety of diseases including cancer, Parkinson's disease, spinal cord injuries, Amyotrophic lateral sclerosis, multiple sclerosis, and muscle damage, amongst a number of other impairments and conditions.[53][54] However, there still exists a great deal of social and scientific uncertainty surrounding stem cell research, which could possibly be overcome through public debate and future research, and further education of the public.
One concern of treatment is the risk that transplanted stem cells could form tumors and become cancerous if cell division continues uncontrollably.[55]
Stem cells are widely studied, for their potential therapeutic use and for their inherent interest.[56]
Supporters of embryonic stem cell research argue that such research should be pursued because the resultant treatments could have significant medical potential. It has been proposed that surplus embryos created for in vitro fertilization could be donated with consent and used for the research.
The recent development of iPS cells has been called a bypass of the legal controversy. Laws limiting the destruction of human embryos have been credited for being the reason for development of iPS cells, but it is still not completely clear whether hiPS cells are equivalent to hES cells. Recent work demonstrates hotspots of aberrant epigenomic reprogramming in hiPS cells (Lister, R., et al., 2011).
Research patents
The patents covering a lot of work on human embryonic stem cells are owned by the Wisconsin Alumni Research Foundation (WARF). WARF does not charge academics to study human stem cells but does charge commercial users. WARF sold Geron Corp. exclusive rights to work on human stem cells but later sued Geron Corp. to recover some of the previously sold rights. The two sides agreed that Geron Corp. would keep the rights to only three cell types. In 2001, WARF came under public pressure to widen access to human stem-cell technology.[57]
A request for reviewing the WARF patents 5,843,780; 6,200,806; 7,029,913 US Patent and Trademark Office were filed by non-profit patent-watchdogs The Foundation for Taxpayer & Consumer Rights, and the Public Patent Foundation as well as molecular biologist Jeanne Loring of the Burnham Institute. According to them, two of the patents granted to WARF are invalid because they cover a technique published in 1993 for which a patent had already been granted to an Australian researcher. Another part of the challenge states that these techniques, developed by James A. Thomson, are rendered obvious by a 1990 paper and two textbooks. Based on this challenge, patent 7,029,913 was rejected in 2010. The two remaining hES WARF patents are due to expire in 2015.
The outcome of this legal challenge is particularly relevant to the Geron Corp. as it can only license patents that are upheld.[58]
Key research events
- 1908: The term "stem cell" was proposed for scientific use by the Russian histologistAlexander Maksimov (1874–1928) at congress of hematologic society in Berlin. It postulated existence of haematopoietic stem cells.
- 1960s: Joseph Altman and Gopal Das present scientific evidence of adult neurogenesis, ongoing stem cell activity in the brain; like André Gernez, their reports contradict Cajal's "no new neurons" dogma and are largely ignored.
- 1963: McCulloch and Till illustrate the presence of self-renewing cells in mouse bone marrow.
- 1968: Bone marrow transplant between two siblings successfully treats SCID.
- 1978: Haematopoietic stem cells are discovered in human cord blood.
- 1981: Mouse embryonic stem cells are derived from the inner cell mass by scientists Martin Evans, Matthew Kaufman, and Gail R. Martin. Gail Martin is attributed for coining the term "Embryonic Stem Cell".
- 1992: Neural stem cells are cultured in vitro as neurospheres.
- 1997: Leukemia is shown to originate from a haematopoietic stem cell, the first direct evidence for cancer stem cells.
- 1998: James Thomson and coworkers derive the first human embryonic stem cell line at theUniversity of Wisconsin–Madison.[59]
- 1998: John Gearhart (Johns Hopkins University) extracted germ cells from fetal gonadal tissue (primordial germ cells) before developing pluripotent stem cell lines from the original extract.
- 2000s: Several reports of adult stem cell plasticity are published.
- 2001: Scientists at Advanced Cell Technology clone first early (four- to six-cell stage) human embryos for the purpose of generating embryonic stem cells.[60]
- 2003: Dr. Songtao Shi of NIH discovers new source of adult stem cells in children's primary teeth.[61]
- 2004–2005: Korean researcher Hwang Woo-Suk claims to have created several humanembryonic stem cell lines from unfertilised human oocytes. The lines were later shown to be fabricated.
- 2005: Researchers at Kingston University in England claim to have discovered a third category of stem cell, dubbed cord-blood-derived embryonic-like stem cells (CBEs), derived from umbilical cord blood. The group claims these cells are able to differentiate into more types of tissue than adult stem cells.
- 2005: Researchers at UC Irvine's Reeve-Irvine Research Center are able to partially restore the ability of rats with paralyzed spines to walk through the injection of human neural stem cells.[62]
- August 2006: Mouse Induced pluripotent stem cells: the journal Cell publishes Kazutoshi Takahashi and Shinya Yamanaka.[63]
- October 2006: Scientists at Newcastle University in England create the first ever artificial liver cells using umbilical cord blood stem cells.[64][65]
- January 2007: Scientists at Wake Forest University led by Dr. Anthony Atala and Harvard University report discovery of a new type of stem cell in amniotic fluid.[66] This may potentially provide an alternative to embryonic stem cells for use in research and therapy.[67]
- June 2007: Research reported by three different groups shows that normal skin cells can be reprogrammed to an embryonic state in mice.[68] In the same month, scientist Shoukhrat Mitalipov reports the first successful creation of a primate stem cell line through somatic cell nuclear transfer[69]
- October 2007: Mario Capecchi, Martin Evans, and Oliver Smithies win the 2007 Nobel Prize for Physiology or Medicine for their work on embryonic stem cells from mice using gene targeting strategies producing genetically engineered mice (known as knockout mice) for gene research.[70]
- November 2007: Human induced pluripotent stem cells: Two similar papers released by their respective journals prior to formal publication: in Cell by Kazutoshi Takahashi and Shinya Yamanaka, "Induction of pluripotent stem cells from adult human fibroblasts by defined factors",[71] and in Science by Junying Yu, et al., from the research group of James Thomson, "Induced pluripotent stem cell lines derived from human somatic cells":[72] pluripotent stem cells generated from mature human fibroblasts. It is possible now to produce a stem cell from almost any other human cell instead of using embryos as needed previously, albeit the risk of tumorigenesis due to c-myc and retroviral gene transfer remains to be determined.
- January 2008: Robert Lanza and colleagues at Advanced Cell Technology and UCSF create the first human embryonic stem cells without destruction of the embryo[73]
- January 2008: Development of human cloned blastocysts following somatic cell nuclear transferwith adult fibroblasts[74]
- February 2008: Generation of pluripotent stem cells from adult mouse liver and stomach: these iPS cells seem to be more similar to embryonic stem cells than the previously developed iPS cells and not tumorigenic, moreover genes that are required for iPS cells do not need to be inserted into specific sites, which encourages the development of non-viral reprogramming techniques.[75]
- March 2008-The first published study of successful cartilage regeneration in the human knee using autologous adult mesenchymal stem cells is published by clinicians from Regenerative Sciences[76]
- October 2008: Sabine Conrad and colleagues at Tübingen, Germany generate pluripotent stem cells from spermatogonial cells of adult human testis by culturing the cells in vitro underleukemia inhibitory factor (LIF) supplementation.[77]
- 30 October 2008: Embryonic-like stem cells from a single human hair.[78]
- 1 March 2009: Andras Nagy, Keisuke Kaji, et al. discover a way to produce embryonic-like stem cells from normal adult cells by using a novel "wrapping" procedure to deliver specific genes to adult cells to reprogram them into stem cells without the risks of using a virus to make the change.[79][80][81] The use of electroporation is said to allow for the temporary insertion of genes into the cell.[82][83][84][85]
- 28 May 2009 Kim et al. announced that they had devised a way to manipulate skin cells to create patient specific "induced pluripotent stem cells" (iPS), claiming it to be the 'ultimate stem cell solution'.[86]
- 11 October 2010 First trial of embryonic stem cells in humans.[87]
- 25 October 2010: Ishikawa et al. write in the Journal of Experimental Medicine that research shows that transplanted cells that contain their new host's nuclear DNA could still be rejected by the invidual's immune system due to foreign mitochondrial DNA. Tissues made from a person's stem cells could therefore be rejected, because mitochondrial genomes tend to accumulate mutations.[88]
- 2011: Israeli scientist Inbar Friedrich Ben-Nun led a team which produced the first stem cells from endangered species, a breakthrough that could save animals in danger of extinction.[89]








No comments:
Post a Comment